Recently we posted this case study.
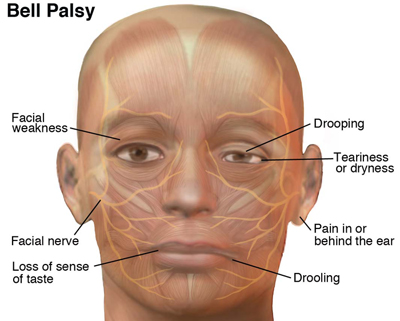
Highly suspicious for Bell’s Palsy (7th cranial, or facial, nerve paralysis). Let’s look at the photo below showing the facial nerve, the facial muscles it innervates, and some common signs/symptoms:
In the case study we saw right-sided paralysis and if you look at the patient’s photo and then at the image above you’ll see the areas on his face which are not working are directly connected to the facial nerve.
Right off the bat it’s important to understand that Bell’s Palsy should be a diagnosis of exclusion. That means you’ve ruled out other reasonable diagnosis and it’s the last one standing. A more serious disorder must first be ruled out.
Always perform a solid neurological exam and stroke screen on these patients as well as a thorough history. Note any other acute neurologic deficit. Bell’s should be isolated just to the facial nerve and should have an onset of under 72 hours. It’s typical to see the onset occur within 48 hours and it can occur overnight as in the case study.
With any acute neurological change we should concern ourselves with the possibility this may be a stroke. Determine that the symptoms are isolated to only one side of the face and follow the pathway of the nerve innervation as seen above. In 60% of cases patients will also report aching around the ear on the affected side and roughly the same percentage of patient’s report an altered sensation of taste. 25% of patient’s report that the ear pain preceded the paralysis by 2-3 days. Include this line of questioning while conducting your exam and history.
A number of other symptoms may be present: tingling, drooling, inability to close the eyelid, and blurred vision.
Focus your exam on the forehead. On the affected side you would expect to see full paralysis when the patient attempts to raise their eyebrows or wrinkle their forehead. In the majority of cases a stroke doesn’t affect this area.
Remember this mnemonic for examining a possible Bell’s Palsy patient:
C – close eyes (orbicularis oculi)
O – open eyes (orbicularis oculi)
W – wrinkle forehead (frontalis)
S – smile (orbicularis oris)
This assesses the major muscles which may be affected: the orbicularis oris (encircling the mouth), the orbicularis oculi (encircling the eye) and the frontalis (the forehead).
The exact cause of Bell’s Palsy isn’t fully understood but it occurs when the 7th cranial nerve becomes infected, swollen, compressed, or damaged. The prognosis is very good and the symptoms typically begin improving within 2 weeks with full resolution at 3-6 months. (Source)
Herpes Simplex infections have been strongly linked to Bell’s Palsy and Ramsey-Hunt Syndrome (varicella zoster virus reactivation) can present in a similar fashion. Examine these patients for a facial rash (specifically around the ear, eyes, and mouth) as this indicates Ramsey-Hunt (shingles). Ramsey-Hunt patients typically have a more severe onset and a harder time recovering. Document and report facial rash as present or as a pertinent negative.
The treatments a physician may consider are antivirals and steroids. For EMS providers recognition, considering and evaluating for a potential code stroke, and conducting a thorough history and physical exam are key. Assessing for, documenting, and reporting findings or negatives such as pain around the ears and rash should be standard practice.









1 Trackback